Four days ago I finished watching the Netflix series ‘13 Reasons Why’ and drafted an opinion piece which I published Monday morning. The show rocked me to my core. So much so, that I landed in the Emergency Room of my local hospital. This is the story of how and why that happened.
 I live with type 1 bipolar disorder. For those who aren’t aware of the various types of bipolar disorder, Bipolar Hope Magazine is an amazing resource and they have an informative section on their website which describes the types of bipolar and different symptoms. In a nutshell, my type of bipolar disorder means that I lean towards the manic side of the condition. If I’m not careful to protect my sleep, I could find myself launching into a manic episode. It doesn’t happen overnight, rather, over the course of several nights of getting little to no sleep.
I live with type 1 bipolar disorder. For those who aren’t aware of the various types of bipolar disorder, Bipolar Hope Magazine is an amazing resource and they have an informative section on their website which describes the types of bipolar and different symptoms. In a nutshell, my type of bipolar disorder means that I lean towards the manic side of the condition. If I’m not careful to protect my sleep, I could find myself launching into a manic episode. It doesn’t happen overnight, rather, over the course of several nights of getting little to no sleep.
As I mentioned in my opinion piece, I put my mental health at risk by choosing to watch the show. I didn’t know how risky it was to begin watching the show because I’ve been mentally healthy for the past 7 years. The last time I was hospitalized for a manic episode was, ironically, exactly seven years ago this month, when I was 5 weeks pregnant with my second child. I thought since I had been so stable for so long, it couldn’t possibly be that risky to watch a few episodes.
I was wrong.
I started watching the show Friday evening, and got through four episodes (binging) before forcing myself to shut it off so that I could get some sleep before flying to Cedar Rapids, Iowa for my nonprofit’s show the following night. Our Iowa Corridor This Is My Brave show was incredibly moving and inspiring, as all of our shows are, and I was so excited to get to spend time with the show’s producers and cast members afterwards. We went out to a local bar and played Cards Against Humanity while eating and hanging out. I had a blast. But unfortunately didn’t get to sleep until 2am EST, and awoke at 6am Sunday morning. I usually sleep well when I’m on the road, but I had so much on my mind having started watching the show the night before and wanting to continue watching.
I pushed play on episode 5 shortly after waking up, and was able to finish the series in the airport on my way home on Sunday. I was furious by the time I finished, and reached out to several of my friends via text to see if they had watched and to get their thoughts. Everyone seemed to have similar feelings, but slightly different reactions. Overall, the few people I was able to connect with directly were shook up by the show, but were glad it was out and was opening the eyes of the public.
At that point I began thinking about those in my circles who were already vulnerable, sensitive. How would they take it if they had watched? How would teenagers react to the show? Especially if they didn’t have solid support systems in place, if they were already in a tough place, if they didn’t have the energy or resources to access proper mental healthcare.
I landed around 8:30pm and grabbed an Uber home. I normally enjoy chatting with the driver, but on this particular ride I needed to connect with one of my close friends. I called my This Is My Brave Co-Founder Anne Marie Ames. She and I have been friends for four years, and I needed to tell her how the show affected me. We talked the entire ride home, and agreed to catch up again during the week.
My husband had let our kids stay up late so they could see me, so I hugged and kissed my little people and got them tucked in by 9pm. My husband knew how I was feeling because I had called him from the airport, and he knew that I wasn’t sleeping well. The plan at that point was to focus on sleep all week, make it a priority again. On the flight home from Chicago I had jotted down my feelings and initial reaction to '13 Reasons Why', and I told him I felt that if I was able to get them organized into a piece that made sense, I’d likely sleep better. I started pulling my thoughts together, tapping away at my laptop, and he went up to bed.
I crawled into bed around midnight, as it had taken me longer than I had hoped to draft my reaction. But I did feel better once I got it out, so I was hopeful I’d be able to get some quality sleep.
Only, instead of crashing and sleeping hard, my sleep was broken and riddled with nightmares. I woke at 5:30am, and since my husband was already downstairs doing his normal early morning workout in the basement, I grabbed and pen and paper and let my feelings flow again. I shot off a draft of my revised piece to two friends and by then it was time to wake the kids and get them off to school.
I recognized my symptoms of hypomania and immediately told my husband that I was going to call my psychiatrist at 8:30am when they opened to get an appointment. He said that he thought that was a good idea and off my family went to work and school. I normally find relief in the calm of the morning once the house is quiet and I’m on my own. But instead I found myself feeling that familiar current of mania beginning to rush through my blood and anxiety creeping in.
I still hoped I could relieve some of these symptoms by publishing my reaction to the show. I felt a little better after hitting Publish on Medium, but things escalated quickly from there.
I picked up my kids from school and took them out for frozen yogurt, one of our favorite treats. I hadn’t seen them all weekend, so it was fun to catch up. As we were sitting there, Kelly, my best friend from college called to see how our Cedar Rapids event had gone. I told her it was amazing, as all our events are, but that I had a lot on my mind. She caught on immediately that I wasn’t in a good place, probably based on the tone of my voice, but I told her I couldn’t talk because of where we were and the kids were with me. She offered to pick up the groceries I said I’d be running out for later that evening, so that I could head to bed early instead. She agreed to meet me back at my place in ½ hour.
{One of the things Kelly asked was critical for her to know how I was doing mentally, and she knows this from being there when my very first manic episode came on back in December of 2005. She asked me where I was on a 10-point scale. I was at a 6-7.}
When a person with type 1 bipolar is at a 6-7, it means that they’re in a hypo-manic state. A person can very quickly go from a 6-7 to a 9-10, meaning they need to be admitted to a psychiatric hospital, if things aren’t addressed in an urgent manner.
Once we were home, I did my best to summarize for Kel why the show '13 Reasons Why' affected me so deeply. She’s a teacher, and hadn’t heard of the show, but when I told her how I had met a friend of mine for coffee that afternoon, she had a better understanding. The friend I met up with had been directly impacted by suicide, as her son Jay took his life last year, and now the family is pursuing a lawsuit because Jay’s guidance counselor had been alerted by a friend three weeks before he took his own life. The counselor had neglected to contact Jay’s parents. You can read about it in the Washington Post.
Little did I know, Kelly had already set an emergency intervention plan into place, even though she may not have noticed it at the time. While she was picking up the groceries for me, she called my husband and let him know that she was concerned about me. She also texted another one of our close friends from college who had a friend who was a pharmacist. (What can I say? It takes a village.)
When Ben got home, he found the kids happily playing video games, while Kelly and I were sitting in the dining room trying to figure out a plan. I needed Ambien to ensure that I got a solid night’s sleep. The only problem was that I hadn’t used a sleep medication in seven years, so we didn’t have anything (expired or otherwise) in the house. We called my psychiatrist’s office to see if we could get through to an after-hours line. We left a message for my doctor’s medical assistant, but by then it was already 6pm and we were running out of time. We called my regular pharmacy, but my psychiatric medication info was out of date. (Side note: I use a mail-order pharmacy to fulfill my regular mood stabilizer prescription which I’ve been on for the past 7 years at the same dose.) The pharmacist at my regular pharmacy recommended an over-the-counter sleep aid, but we weren’t convinced that would work for me given my level of hypomania.
Our friend who is the pharmacist (in California) communicated by text that if I didn’t have Ambien on hand at home, I would need to go to the Emergency Room to get a prescription for it, and that was what she recommended given my symptoms. I argued it was overreacting, but based on my experience living with this condition for eleven years now, and my past 4 psychiatric hospitalizations for mania, I also knew she was right.
Kelly offered to drive me to the hospital while Ben held down the fort at home. I resisted at first, as it seemed dramatic and unnecessary. I wanted to just get an OTC sleep med, and said we could get Ambien the next day from my psychiatrist. But looking back now, it's a good thing I didn't resist as I could have ended up in handcuffs again, being carted off to the Emergency Room and then the psychiatric hospital. I didn't want my kids to have to see that happen, so I happily went along with the intervention plan.
We joked on the drive over about how efficient my intervention team was and how I was voting her President of the team based on her stellar performance. (In college, Kelly was President of the water polo team and I was Vice President, so it seemed fitting.) We were immediately admitted to the ER, the intake nurse took my vitals, and I was sent back to a triage room with a bed. By that point I had called my parents to let them know what was going on, letting them know the plan and that we had everything under control. They were worried but relieved, and asked that I keep them posted.
The ER doc was really great, and got us in and out quickly with a script for the Ambien that hopefully would do the trick and get me through until I saw my psychiatrist on Wednesday. Ben had called his mom and she was already at our house by the time I was getting my discharge papers, and he met us at the hospital right as I was released so that he could drive me to get my script and Kelly could head home to her family.
Ben’s mom got the kids in bed as I called my parents to update them once we got home around 8:30pm. I ate a little something for dinner, and was crawling into bed by 9:30, ready to let the meds do their trick and lull me into a deep sleep.
Only it didn’t exactly work as planned.
I slept from 10pm until I woke at 1:30am, unable to get back to sleep. Hypomania/mania has a way of doing that to a person. I woke my husband and told him I couldn’t sleep, so I took another dose of the sleep med. I woke groggy at 6am Tuesday morning. Concerned that I had to take two doses, when in the past one dose had worked for me, we called to bump up my psychiatrist appointment, and luckily she had a slot in her schedule for Tuesday afternoon.
My husband was able to take time off from work to drive me to my psychiatrist appointment. We filled her in on everything that had happened, and made a new plan including medication changes. She provided us with her emergency contact info in case we needed it, and answered all our questions. We were in and out in an hour total. My mother-in-law was able to help us with our kids while my husband went back to work for the afternoon and I went to run a few necessary errands, including picking up my new prescription. My therapist (who I haven’t seen since December, because I’ve been “busy”), has an awesome online scheduling tool for current clients. I grabbed one of her only two open appointment slots for Thursday.
Tuesday night we followed the plan. It was extremely difficult to get out of bed Wednesday morning due to the side effects of the medication changes. I haven’t had trouble getting out of bed because of my mental illness for so many years that I forgot what it felt like. It’s hell.
My anxiety has returned due to this “almost-episode,” which is totally normal. It’s just been so long since I’ve felt it that it’s been a little overwhelming. Uncomfortable, yes. Manageable, yes. Especially when I have such an incredible support system and so many resources at my fingertips.
I may have been able to stay mentally healthy for seven years, and yes, that's a long streak. But if this week has taught me anything it's that I'm not immune to relapses. I live with type 1 bipolar disorder and I'll always have it. Like any other chronic condition, it's lifelong. I'll continue to kick bipolar's ass, I know I will. I'm even a little grateful for this week's experience because I had been feeling like a bit of an imposter lately, having not felt symptoms for so long and getting to do this nonprofit work where I hear stories of individuals overcoming mental illness every week. I'll forever be a member of the club, my tribe, as I call it. And together we're ending the stigma surrounding mental health disorders. One true story at a time.
*****
About a year ago, I wrote a guest post for a website called OC87Recovery Diaries, and in it, I stated that we didn’t have a plan. The reason I’m publishing this post is not to highlight how fortunate I am, but to point out how I almost landed in a psychiatric hospital this week, but didn’t, because we had a plan. It may not have been a formal, executed WRAP (Wellness Recovery Action Plan), but it was darn near close, and it worked.
If you or someone you love lives with a mental illness, it's important to have a plan. And if you're in a tough place right now - here are some things I find helpful:
- Know your local and national mental health resources, including the crisis hotlines. This Is My Brave's Resources page is a great place to look, or even just Google it and keep that info handy.
- Make sure you know how to contact your psychiatrist after-hours in case of emergency.
- Keep a journal that lists the meds you're currently taking and what's working for you. Allow those closest to you to have access to this in case of emergency.
- Don't be afraid to be completely honest about how you're feeling. Feeling overwhelmed, triggered, fragile, etc., and sharing your feelings with those you trust is NOT weakness. In fact, it's the complete opposite. It's brave to allow yourself to be that vulnerable and it leads to deeper, more close-knit relationships with the people you love.
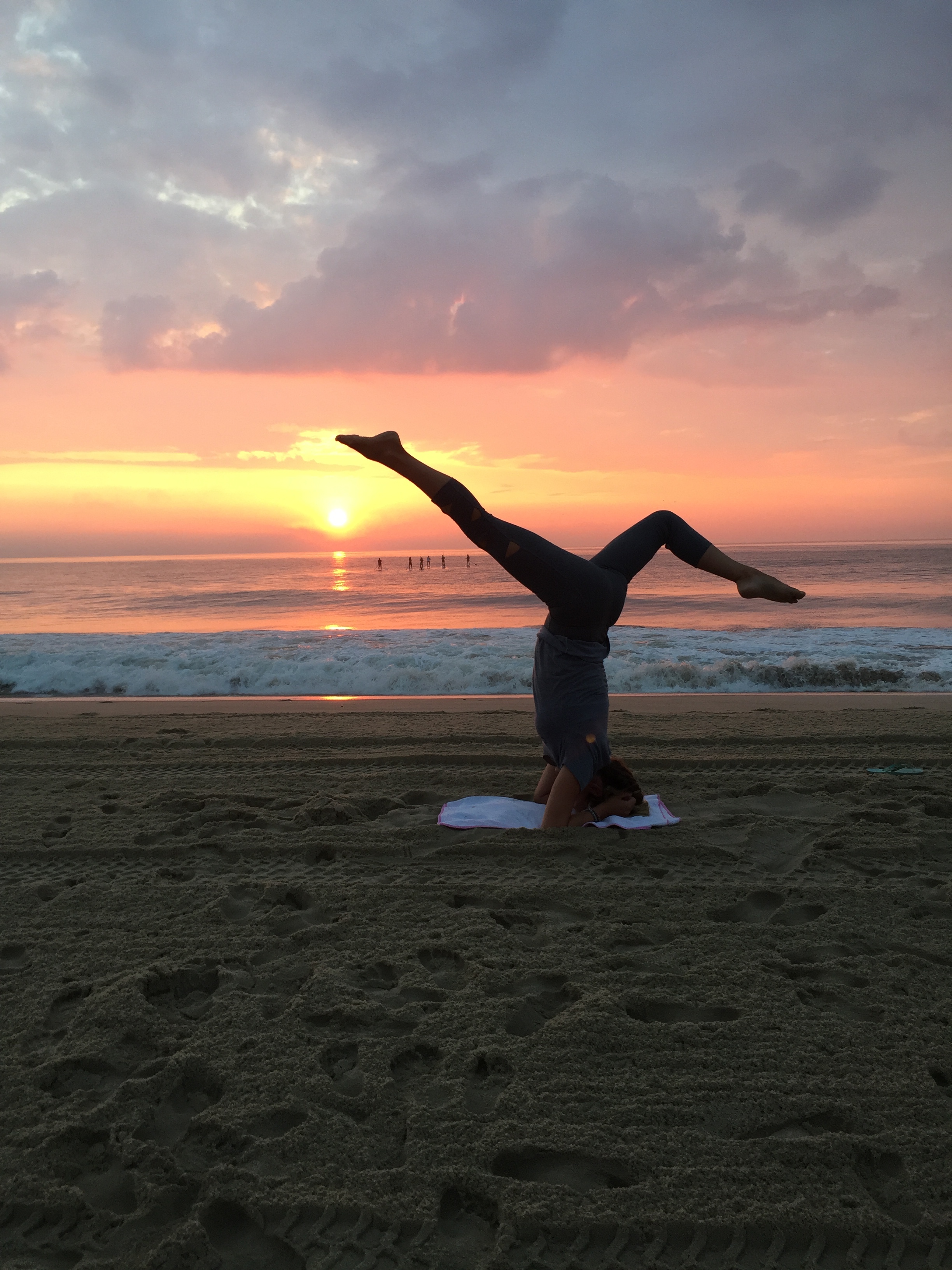
- Don't lose sight of self-care. We often get so wrapped up in our day-to-day lives that we forget to take time out for ourselves, and being too "busy" can lead to burn-out and mental health issues.